In our fight against infectious diseases, antimicrobials have stood as essential allies, spanning antibiotics, antivirals, antifungals, and antiparasitics. They’ve been pivotal in safeguarding human, animal, and plant health. Yet, a looming threat shadows their efficacy— Antimicrobial Resistance (AMR). This evolutionary survival tactic among bacteria, viruses, fungi, and parasites renders our remedies ineffective. This escalates disease transmission risks and threatening dire outcomes, from disabilities to fatalities.

AMR isn’t just a product of nature; it’s an accelerated consequence of human actions, particularly the misuse and overuse of these essential medicines. General practitioners often prescribe antibiotics excessively, even in the absence of clear indications. Hence perpetuating the perception of antibiotics as panaceas for all ailments. Rampant antibiotic use in developing countries, stemming from easy accessibility without prescription, further compounds this issue. The intensive and prolonged use of antimicrobials within hospital settings stands as a significant catalyst for highly resistant infections, accentuated by factors like lengthy hospital stays and unchecked infection spread.
“In many developing countries, excessive use is due to the easy availability of antimicrobial drugs that can be purchased without prescription of a physician or other qualified health professional”
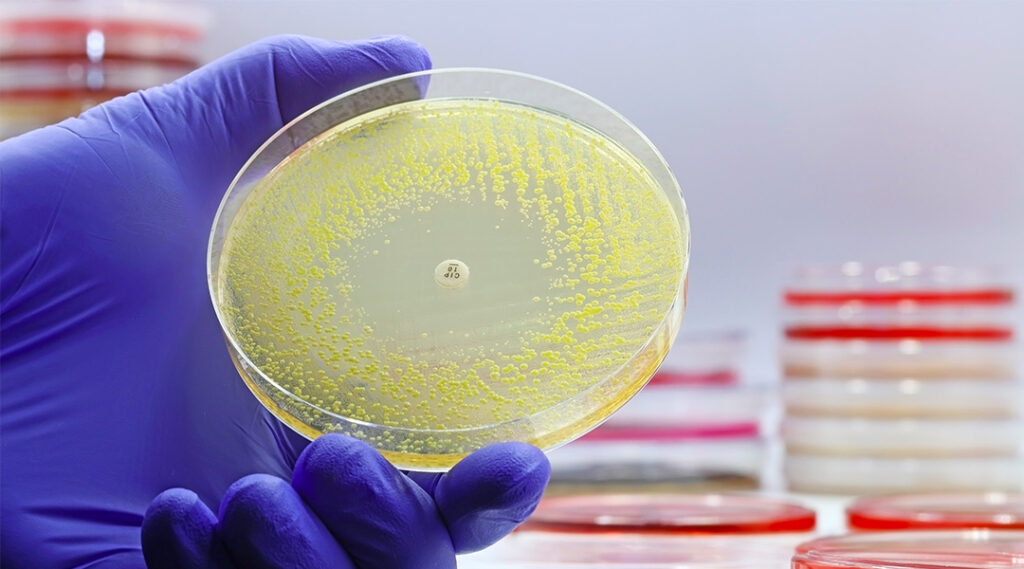
AMR and Human Infections
Public misconceptions about antibiotics’ efficacy against common illnesses and prevalent self-medication practices significantly contribute to inadequate dosing and microbial adaptation. The extensive use of antibiotics in food-producing animals and aquaculture further compounds the global resistance problem. Environmental factors also play a crucial role, with soil serving as a reservoir for antibiotic resistance genes and water acting as a medium for bacterial dissemination.
This global challenge jeopardizes the very core of modern medicine, influencing everyday treatments and critical procedures like chemotherapy and surgeries. Its ripple effects extend to animal and plant health, impacting agricultural productivity and food security.
Tha State of AMR in the World
The recent Global Antimicrobial Resistance and Use Surveillance System (GLASS) report unveiled alarming rates of antibiotic resistance in prevalent bacterial pathogens such as E. coli and methicillin-resistant Staphylococcus aureus. Concurrently, the emergence of multi-drug resistant fungi, like Candida auris, poses formidable obstacles, especially when infections coincide with conditions like HIV.

The intricate relationship between AMR and diseases such as HIV, tuberculosis (TB), malaria, and neglected tropical diseases (NTDs) reveals further complexities. HIV drug resistance heightens infection rates, complicating treatment. Multidrug-resistant TB strains strain healthcare systems, while drug-resistant parasites challenge malaria control, necessitating vigilant monitoring and innovative strategies.
The Impact of Antimicrobial Resistance
The World Health Organization (WHO) has long championed a concerted global effort to contain AMR. Initiatives like the Global Strategy for Containment of Antimicrobial Resistance (2001) and “The Evolving Threat of Antimicrobial Resistance – Options for Action” (2012) propose multifaceted interventions, spanning health system strengthening, enhanced surveillance, optimized antimicrobial usage, infection prevention, and new drug and vaccine development.
Surveillance plays a pivotal role in this landscape. WHO’s global report on AMR highlighted the utility of surveillance data in informing treatment choices, understanding resistance trends, and pinpointing priority areas for interventions. Yet, significant gaps persist in surveillance efforts across many parts of the world, impeding a comprehensive understanding of the distribution and extent of this phenomenon.
Challenges Encountered when Tackling AMR
Moreover, the economic fallout of antibiotic resistance presents a multifaceted challenge. Encompassing increased healthcare costs, longer hospital stays, and societal costs linked to productivity losses and mortality. While estimates from Europe and the US put forth staggering figures in billions. These assessments likely underrepresent the evolving burden of antibiotic resistance.
The intricate interplay of societal, healthcare, agricultural, and environmental factors underscores the complexity of combating antibiotic resistance. It urges comprehensive, globally coordinated efforts to curb this burgeoning global health crisis. Join the global movement against AMR—spread awareness, support research, advocate for responsible antibiotic use, and be a part of the solution in safeguarding our collective health.
Efforts to Betake Antimicrobial Resistance
In the face of this crisis, a unified, cross-sectoral One Health approach emerges as a guiding light. The Global Action Plan (GAP) on Antimicrobial Resistance serves as a blueprint, urging countries to craft national action plans prioritizing One Health perspectives. Collaborative efforts, spearheaded by the Quadripartite Joint Secretariat on Antimicrobial Resistance (comprising WHO, FAO, UNEP, and OIE), foster global and regional initiatives to combat this crisis.
Critical events like World AMR Awareness Week (WAAW) and the formulation of national action plans underscore the urgent need for sustained progress, strong governance, and resource mobilization. Strategic interventions—antimicrobial stewardship, surveillance systems like GLASS, and WHO core interventions—emphasize the need for optimized antimicrobial usage and equitable healthcare access.

Immediate Action is Needed
However, significant challenges persist. Diminishing pipelines for new antimicrobials and shortages of generic antibiotics. Collaborations with organizations like GARDP and initiatives advocating for innovation and investment remain pivotal in bridging these research and development gaps.
The urgency of addressing AMR, especially antibiotic resistance in bacteria, cannot be overstated. Over decades, bacteria causing various infections have steadily developed resistance to new antibiotics. This heralds a global healthcare crisis that demands immediate action.
References
Antimicrobial resistance: a global multifaceted phenomenon. 2015. Pathog Glob Health.
Antimicrobial Resistance Collaborators. 2022. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis.
Five reasons to care about antimicrobial resistance (AMR). 2023. Council of the European Union.
Antimicrobial resistance. 2023. World Health Organization.